Skin Cancer Treatment (PDQ®): Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
General Information About Skin Cancer
Skin cancer is a disease in which malignant (cancer) cells form in the tissues of the skin.
The skin is the body's largest organ. It protects against heat, sunlight, injury, and infection. Skin also helps control body temperature and stores water, fat, and vitamin D. The skin has several layers, but the two main layers are the epidermis (upper or outer layer) and the dermis (lower or inner layer). Skin cancer begins in the epidermis, which is made up of three kinds of cells:
- Squamous cells: Thin, flat cells that form the top layer of the epidermis.
- Basal cells: Round cells under the squamous cells.
- Melanocytes: Cells that make melanin and are found in the lower part of the epidermis. Melanin is the pigment that gives skin its natural color. When skin is exposed to the sun, melanocytes make more pigment and cause the skin to darken.
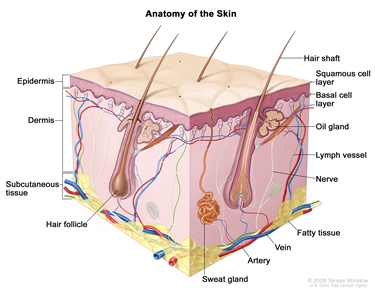
Anatomy of the skin showing the epidermis (including the squamous cell and basal cell layers), dermis, subcutaneous tissue, and other parts of the skin.
Skin cancer can occur anywhere on the body, but it is most common in skin that is often exposed to sunlight, such as the face, neck, and hands.
Different types of cancer start in the skin.
Skin cancer may form in basal cells or squamous cells. Basal cell carcinoma and squamous cell carcinoma are the most common types of skin cancer. They are also called nonmelanoma skin cancer. Actinic keratosis is a skin condition that sometimes becomes squamous cell carcinoma.
Melanoma is less common than basal cell carcinoma or squamous cell carcinoma. It is more likely to invade nearby tissues and spread to other parts of the body.
This summary is about basal cell carcinoma, squamous cell carcinoma of the skin, and actinic keratosis.
Having a fair complexion and being exposed to sunlight are risk factors for basal cell carcinoma and squamous cell carcinoma of the skin.
Anything that increases a person's chance of getting a disease is called a risk factor. Not every person with one or more of these risk factors will develop skin cancer, and it will develop in people who don't have any known risk factors. Talk with your doctor if you think you may be at risk.
Risk factors for basal cell carcinoma and squamous cell carcinoma of the skin include the following:
- Being exposed to natural sunlight or artificial sunlight (such as from tanning beds) over long periods of time.
- Having a fair complexion, which includes the following:
- Fair skin that freckles and burns easily, does not tan, or tans poorly.
- Blue, green, or other light-colored eyes.
- Red or blond hair.
Although having a fair complexion is a risk factor for skin cancer, people of all skin colors can get skin cancer.
- Having a history of sunburns.
- Having a personal or family history of basal cell carcinoma, squamous cell carcinoma of the skin, actinic keratosis, familial dysplastic nevus syndrome, or unusual moles.
- Having certain changes in the genes or hereditary syndromes, such as basal cell nevus syndrome, that are linked to skin cancer.
- Having skin inflammation that has lasted for long periods of time.
- Having a weakened immune system.
- Being exposed to arsenic.
- Past treatment with radiation.
Older age is the main risk factor for most cancers. The chance of getting cancer increases as you get older.
Basal cell carcinoma, squamous cell carcinoma of the skin, and actinic keratosis often appear as a change in the skin.
Not all changes in the skin are a sign of basal cell carcinoma, squamous cell carcinoma of the skin, or actinic keratosis. Check with your doctor if you notice any changes in your skin.
Signs of basal cell carcinoma and squamous cell carcinoma of the skin include the following:
- A sore that does not heal.
- Areas of the skin that are:
- Raised, smooth, shiny, and look pearly.
- Firm and look like a scar, and may be white, yellow, or waxy.
- Raised and red or reddish-brown.
- Scaly, bleeding, or crusty.
Basal cell carcinoma and squamous cell carcinoma of the skin occur most often in areas of the skin exposed to the sun, such as the nose, ears, lower lip, or top of the hands.
Signs of actinic keratosis include the following:
- A rough, red, pink, or brown, scaly patch on the skin that may be flat or raised.
- Cracking or peeling of the lower lip that is not helped by lip balm or petroleum jelly.
Actinic keratosis occurs most commonly on the face or the top of the hands.
Tests or procedures that examine the skin are used to diagnose basal cell carcinoma and squamous cell carcinoma of the skin.
In addition to asking about your personal and family health history and doing a physical exam, your doctor may perform the following tests and procedures:
- Skin exam: An exam of the skin for bumps or spots that look abnormal in color, size, shape, or texture.
-
Skin biopsy: All or part of the abnormal-looking growth is cut from the skin and viewed under a microscope by a pathologist to check for signs of cancer. There are four main types of skin biopsies:
- Shave biopsy: A sterile razor blade is used to "shave-off" the abnormal-looking growth.
- Punch biopsy: A special instrument called a punch or a trephine is used to remove a circle of tissue from the abnormal-looking growth.
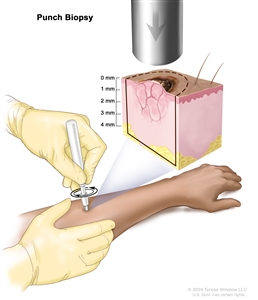
Punch biopsy. A sharp, hollow, circular instrument is used to remove a small, round piece of tissue from a lesion on the skin. The instrument is turned clockwise and counterclockwise to cut about 4 millimeters (mm) down to the layer of fatty tissue below the skin and remove the sample of tissue. Skin thickness is different on different parts of the body. - Incisional biopsy: A scalpel is used to remove part of a growth.
- Excisional biopsy: A scalpel is used to remove the entire growth.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis for squamous cell carcinoma of the skin depends mostly on the following:
- Stage of the cancer.
- Whether the patient is immunosuppressed.
- Whether the patient uses tobacco.
- The patient's general health.
Treatment options for basal cell carcinoma and squamous cell carcinoma of the skin depend on the following:
- The type of cancer.
- The stage of the cancer, for squamous cell carcinoma.
- The size of the tumor and what part of the body it affects.
- The patient's general health.
Stages of Skin Cancer
After squamous cell cancer of the skin has been diagnosed, tests are done to find out if cancer cells have spread within the skin or to other parts of the body.
The process used to find out if cancer has spread within the skin or to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the stage in order to plan treatment for squamous cell carcinoma of the skin.
Basal cell carcinoma of the skin rarely spreads to other parts of the body. Staging tests to check whether basal cell carcinoma of the skin has spread are usually not needed.
The following tests and procedures may be used in the staging process for squamous cell carcinoma of the skin:
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, such as the head, neck, and chest, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- PET scan (positron emission tomography scan): A procedure to find malignant tumor cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells do. Sometimes a PET scan and CT scan are done at the same time.
- Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues, such as lymph nodes, or organs and make echoes. The echoes form a picture of body tissues called a sonogram. The picture can be printed to be looked at later. An ultrasound exam of the regional lymph nodes may be done for basal cell carcinoma and squamous cell carcinoma of the skin.
- Eye exam with dilated pupil: An exam of the eye in which the pupil is dilated (opened wider) with medicated eye drops to allow the doctor to look through the lens and pupil to the retina and optic nerve. The inside of the eye, including the retina and the optic nerve, is examined with a light.
- Lymph node biopsy: The removal of all or part of a lymph node. A pathologist views the lymph node tissue under a microscope to check for cancer cells. A lymph node biopsy may be done for squamous cell carcinoma of the skin.
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
Cancer may spread from where it began to other parts of the body.
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began (the primary tumor) and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor (metastatic tumor) in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumor (metastatic tumor) in another part of the body.
The metastatic tumor is the same type of cancer as the primary tumor. For example, if skin cancer spreads to the lung, the cancer cells in the lung are actually skin cancer cells. The disease is metastatic skin cancer, not lung cancer.
Staging for basal cell carcinoma and squamous cell carcinoma of the skin depends on where the cancer formed.
Staging for basal cell carcinoma and squamous cell carcinoma of the eyelid is different from staging for basal cell carcinoma and squamous cell carcinoma found on other areas of the head or neck. There is no staging system for basal cell carcinoma or squamous cell carcinoma that is not found on the head or neck.
Surgery to remove the primary tumor and abnormal lymph nodes is done so that tissue samples can be studied under a microscope. This is called pathologic staging and the findings are used for staging as described below. If staging is done before surgery to remove the tumor, it is called clinical staging. The clinical stage may be different from the pathologic stage.
The following stages are used for basal cell carcinoma and squamous cell carcinoma of the skin that is on the head or neck but not on the eyelid:
Stage 0 (Carcinoma in situ)
In stage 0, abnormal cells are found in the squamous cell or basal cell layer of the epidermis. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is also called carcinoma in situ.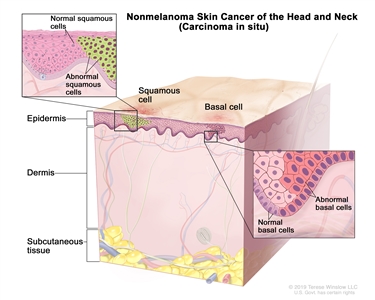
Nonmelanoma skin cancer of the head and neck (carcinoma in situ). Abnormal cells are found in the squamous cell or basal cell layer of the epidermis. These abnormal cells may become cancer and spread into nearby normal tissue.
Stage I
In stage I, cancer has formed and the tumor is 2 centimeters or smaller.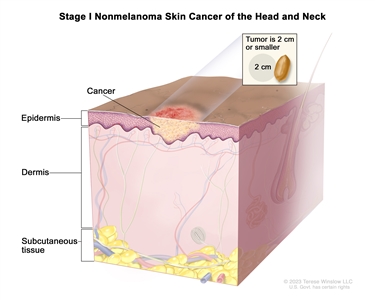
Stage I nonmelanoma skin cancer of the head and neck. The tumor is 2 centimeters or smaller.
Stage II
In stage II, the tumor is larger than 2 centimeters but not larger than 4 centimeters.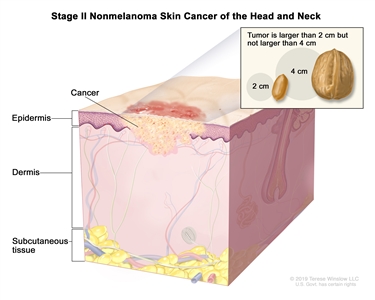
Stage II nonmelanoma skin cancer of the head and neck. The tumor is larger than 2 centimeters but not larger than 4 centimeters.
Stage III
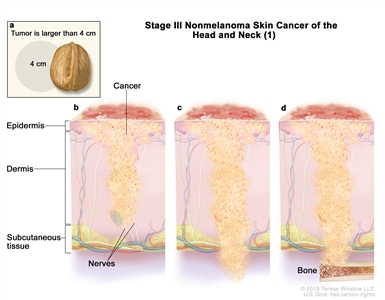
Stage III nonmelanoma skin cancer of the head and neck (1). The tumor is (a) larger than 4 centimeters; or cancer has spread to (b) tissue covering the nerves below the dermis; or (c) below the subcutaneous tissue; or (d) the bone and the bone has minor damage. Cancer may have spread to one lymph node on the same side of the body as the tumor and the node is 3 centimeters or smaller, and cancer has not spread through to the outside covering of the lymph node (not shown).
or
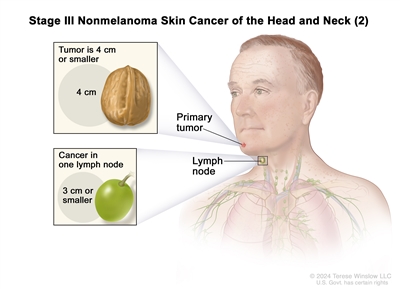
Stage III nonmelanoma skin cancer of the head and neck (2). The tumor is 4 centimeters or smaller. Cancer has spread to one lymph node on the same side of the body as the tumor and the node is 3 centimeters or smaller.
In stage III, one of the following is found:
- the tumor is larger than 4 centimeters, or cancer has spread to tissue covering the nerves below the dermis, or has spread below the subcutaneous tissue, or has spread to the bone and the bone has minor damage. Cancer may have also spread to one lymph node on the same side of the body as the tumor and the node is 3 centimeters or smaller, and cancer has not spread through to the outside covering of the lymph node; or
- the tumor is 4 centimeters or smaller. Cancer has spread to one lymph node on the same side of the body as the tumor and the node is 3 centimeters or smaller.
Stage IV
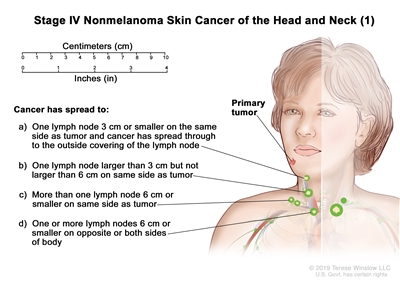
Stage IV nonmelanoma skin cancer of the head and neck (1). The tumor is any size. Cancer may have spread to the bone and the bone has minor damage, or to tissue covering the nerves below the dermis, or below the subcutaneous tissue. Cancer has spread to: (a) one lymph node on the same side of the body as the tumor, the node is 3 centimeters or smaller, and cancer has spread through to the outside covering of the lymph node; or (b) one lymph node on the same side of the body as the tumor, the node is larger than 3 centimeters but not larger than 6 centimeters, and cancer has not spread through to the outside covering of the lymph node; or (c) more than one lymph node on the same side of the body as the tumor, the nodes are 6 centimeters or smaller, and cancer has not spread through to the outside covering of the lymph nodes; or (d) one or more lymph nodes on the opposite side of the body as the tumor or on both sides of the body, the nodes are 6 centimeters or smaller, and cancer has not spread through to the outside covering of the lymph nodes.
or
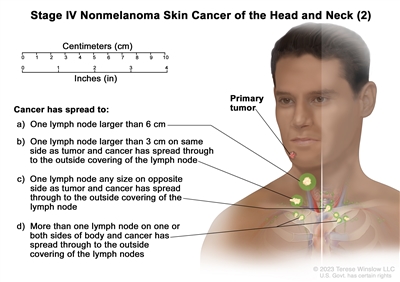
Stage IV nonmelanoma skin cancer of the head and neck (2). The tumor is any size and cancer has spread to: (a) one lymph node that is larger than 6 centimeters and cancer has not spread through to the outside covering of the lymph node; or (b) one lymph node on the same side of the body as the tumor, the affected node is larger than 3 centimeters, and cancer has spread through to the outside covering of the lymph node; or (c) one lymph node on the opposite side of the body as the tumor, the affected node is any size, and cancer has spread through to the outside covering of the lymph node; or (d) more than one lymph node on one or both sides of the body and cancer has spread through to the outside covering of the lymph nodes.
or
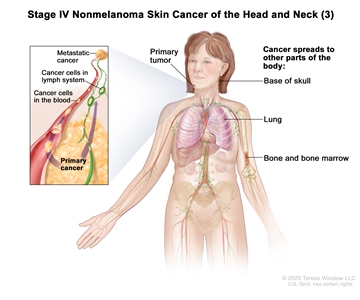
Stage IV nonmelanoma skin cancer of the head and neck (3). The tumor is any size and cancer has spread to bone marrow or to bone, including the base of the skull, and the bone has been damaged; or cancer has spread to other parts of the body, such as the lung.
In stage IV, one of the following is found:
- the tumor is any size and cancer may have spread to the bone and the bone has minor damage, or to tissue covering the nerves below the dermis, or below the subcutaneous tissue. Cancer has spread to the lymph nodes as follows:
- one lymph node on the same side of the body as the tumor, the affected node is 3 centimeters or smaller, and cancer has spread through to the outside covering of the lymph node; or
- one lymph node on the same side of the body as the tumor, the affected node is larger than 3 centimeters but not larger than 6 centimeters, and cancer has not spread through to the outside covering of the lymph node; or
- more than one lymph node on the same side of the body as the tumor, the affected nodes are 6 centimeters or smaller, and cancer has not spread through to the outside covering of the lymph nodes; or
- one or more lymph nodes on the opposite side of the body as the tumor or on both sides of the body, the affected nodes are 6 centimeters or smaller, and cancer has not spread through to the outside covering of the lymph nodes.
- the tumor is any size and cancer may have spread to tissue covering the nerves below the dermis, or below the subcutaneous tissue, or to bone marrow or to bone, including the bottom of the skull. Also:
- cancer has spread to one lymph node that is larger than 6 centimeters and cancer has not spread through to the outside covering of the lymph node; or
- cancer has spread to one lymph node on the same side of the body as the tumor, the affected node is larger than 3 centimeters, and cancer has spread through to the outside covering of the lymph node; or
- cancer has spread to one lymph node on the opposite side of the body as the tumor, the affected node is any size, and cancer has spread through to the outside covering of the lymph node; or
- cancer has spread to more than one lymph node on one or both sides of the body and cancer has spread through to the outside covering of the lymph nodes.
- the tumor is any size and cancer has spread to bone marrow or to bone, including the bottom of the skull, and the bone has been damaged. Cancer may have also spread to the lymph nodes; or
- cancer has spread to other parts of the body, such as the lung.
The following stages are used for basal cell carcinoma and squamous cell carcinoma of the skin on the eyelid:
Stage 0 (Carcinoma in situ)
In stage 0, abnormal cells are found in the epidermis, usually in the basal cell layer. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is also called carcinoma in situ.
Stage I
In stage I, cancer has formed. Stage I is divided into stages IA and IB.
- Stage IA: The tumor is 10 millimeters or smaller and may have spread to the edge of the eyelid where the lashes are, to the connective tissue in the eyelid, or to the full thickness of the eyelid.
- Stage IB: The tumor is larger than 10 millimeters but not larger than 20 millimeters and the tumor has not spread to the edge of the eyelid where the lashes are, or to the connective tissue in the eyelid.
Stage II
Stage II is divided into stages IIA and IIB.
- In stage IIA, one of the following is found:
- the tumor is larger than 10 millimeters but not larger than 20 millimeters and has spread to the edge of the eyelid where the lashes are, to the connective tissue in the eyelid, or to the full thickness of the eyelid; or
- the tumor is larger than 20 millimeters but not larger than 30 millimeters and may have spread to the edge of the eyelid where the lashes are, to the connective tissue in the eyelid, or to the full thickness of the eyelid.
- In stage IIB, the tumor may be any size and has spread to the eye, eye socket, sinuses, tear ducts, or brain, or to the tissues that support the eye.
Stage III
Stage III is divided into stages IIIA and IIIB.
- Stage IIIA: The tumor may be any size and may have spread to the edge of the eyelid where the lashes are, to the connective tissue in the eyelid, or to the full thickness of the eyelid, or to the eye, eye socket, sinuses, tear ducts, or brain, or to the tissues that support the eye. Cancer has spread to one lymph node on the same side of the body as the tumor and the node is 3 centimeters or smaller.
- Stage IIIB: The tumor may be any size and may have spread to the edge of the eyelid where the lashes are, to the connective tissue in the eyelid, or to the full thickness of the eyelid, or to the eye, eye socket, sinuses, tear ducts, or brain, or to the tissues that support the eye. Cancer has spread to lymph nodes as follows:
- one lymph node on the same side of the body as the tumor and the node is larger than 3 centimeters; or
- more than one lymph node on the opposite side of the body as the tumor or on both sides of the body.
Stage IV
In stage IV, the tumor has spread to other parts of the body, such as the lung or liver.
Treatment depends on the type of skin cancer or other skin condition diagnosed:
Basal cell carcinoma

Basal cell carcinoma. A skin cancer lesion that looks reddish brown and slightly raised (left panel) and a skin cancer lesion that looks like an open sore with a pearly rim (right panel).
Basal cell carcinoma is the most common type of skin cancer. It usually occurs on areas of the skin that have been in the sun, most often the nose. Often this cancer appears as a raised bump that looks smooth and pearly. A less common type looks like a scar or it is flat and firm and may be skin-colored, yellow, or waxy. Basal cell carcinoma may spread to tissues around the cancer, but it usually does not spread to other parts of the body.
Squamous cell carcinoma
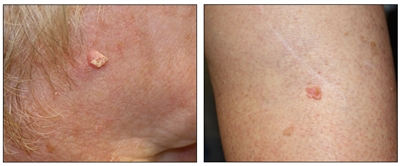
Squamous cell carcinoma. A skin cancer lesion on the face that looks raised and crusty (left panel) and a skin cancer lesion on the leg that looks pink and raised (right panel).
Squamous cell carcinoma occurs on areas of the skin that have been damaged by the sun, such as the ears, lower lip, and the back of the hands. Squamous cell carcinoma may also appear on areas of the skin that have been sunburned or exposed to chemicals or radiation. Often this cancer looks like a firm red bump. The tumor may feel scaly, bleed, or form a crust. Squamous cell tumors may spread to nearby lymph nodes. Squamous cell carcinoma that has not spread can usually be cured.
Actinic keratosis
Actinic keratosis is a skin condition that is not cancer, but sometimes changes into squamous cell carcinoma. One or more lesions may occur in areas that have been exposed to the sun, such as the face, the back of the hands, and the lower lip. It looks like rough, red, pink, or brown scaly patches on the skin that may be flat or raised, or as a cracked and peeling lower lip that is not helped by lip balm or petroleum jelly. Actinic keratosis may disappear without treatment.
Treatment Option Overview
There are different types of treatment for patients with basal cell carcinoma, squamous cell carcinoma of the skin, and actinic keratosis.
Different types of treatment are available for patients with basal cell carcinoma, squamous cell carcinoma of the skin, and actinic keratosis. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
The following types of treatment are used:
Surgery
One or more of the following surgical procedures may be used to treat basal cell carcinoma, squamous cell carcinoma of the skin, or actinic keratosis:
- Simple excision: The tumor, along with some of the normal tissue around it, is cut from the skin.
- Mohs micrographic surgery: The tumor is cut from the skin in thin layers. During the procedure, the edges of the tumor and each layer of tumor removed are viewed through a microscope to check for cancer cells. Layers continue to be removed until no more cancer cells are seen. This type of surgery removes as little normal tissue as possible. It is often used to remove skin cancer on the face, fingers, or genitals and skin cancer that does not have a clear border.
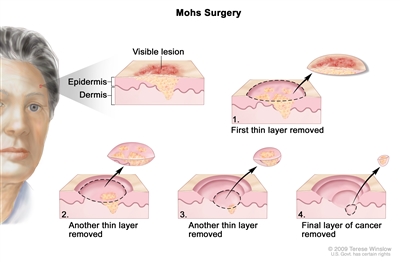
Mohs surgery. A surgical procedure to remove skin cancer in several steps. First, a thin layer of cancerous tissue is removed. Then, a second thin layer of tissue is removed and viewed under a microscope to check for cancer cells. More layers are removed one at a time until the tissue viewed under a microscope shows no remaining cancer. This type of surgery is used to remove as little normal tissue as possible and is often used to remove skin cancer on the face. - Shave excision: The abnormal area is shaved off the surface of the skin with a small blade.
- Curettage and electrodesiccation: The tumor is cut from the skin with a curette (a sharp, spoon-shaped tool). A needle-shaped electrode is then used to treat the area with an electric current that stops the bleeding and destroys cancer cells that remain around the edge of the wound. The process may be repeated one to three times during the surgery to remove all of the cancer. This type of treatment is also called electrosurgery.
- Cryosurgery: A treatment that uses an instrument to freeze and destroy abnormal tissue, such as carcinoma in situ. This type of treatment is also called cryotherapy.
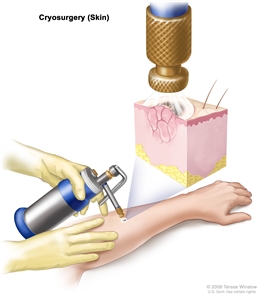
Cryosurgery. An instrument with a nozzle is used to spray liquid nitrogen or liquid carbon dioxide to freeze and destroy abnormal tissue. - Laser surgery: A surgical procedure that uses a laser beam (a narrow beam of intense light) as a knife to make bloodless cuts in tissue or to remove a surface lesion such as a tumor.
- Dermabrasion: Removal of the top layer of skin using a rotating wheel or small particles to rub away skin cells.
Simple excision, Mohs micrographic surgery, curettage and electrodesiccation, and cryosurgery are used to treat basal cell carcinoma and squamous cell carcinoma of the skin. Laser surgery is rarely used to treat basal cell carcinoma. Simple excision, shave excision, curettage and desiccation, dermabrasion, and laser surgery are used to treat actinic keratosis.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer.
External radiation therapy is used to treat basal cell carcinoma and squamous cell carcinoma of the skin.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing.
Chemotherapy for basal cell carcinoma, squamous cell carcinoma of the skin, and actinic keratosis is usually topical (applied to the skin in a cream or lotion). Topical fluorouracil (5-FU) is used to treat basal cell carcinoma.
See Drugs Approved for Basal Cell Carcinoma for more information.
Photodynamic therapy
Photodynamic therapy (PDT) is a cancer treatment that uses a drug and a certain type of light to kill cancer cells. A drug that is not active until it is exposed to light is injected into a vein or put on the skin. The drug collects more in cancer cells than in normal cells. For skin cancer, laser light is shined onto the skin and the drug becomes active and kills the cancer cells. Photodynamic therapy causes little damage to healthy tissue.
Photodynamic therapy is also used to treat actinic keratoses.
Immunotherapy
Immunotherapy is a treatment that uses the patient's immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body's natural defenses against cancer.
There are different types of immunotherapy used to treat skin cancer:
- Immune checkpoint inhibitors block proteins called checkpoints that are made by some types of immune system cells, such as T cells, and some cancer cells. PD-1 is a protein on the surface of T cells that helps keep the body's immune responses in check. PD-L1 is a protein found on some types of cancer cells. When PD-1 attaches to PD-L1, it stops the T cell from killing the cancer cell. PD-1 and PD-L1 inhibitors keep PD-1 and PD-L1 proteins from attaching to each other. This allows the T cells to kill cancer cells.
- Cemiplimab and pembrolizumab are types of PD-1 inhibitors used to treat squamous cell carcinoma of the skin that is locally advanced or has spread to other parts of the body.
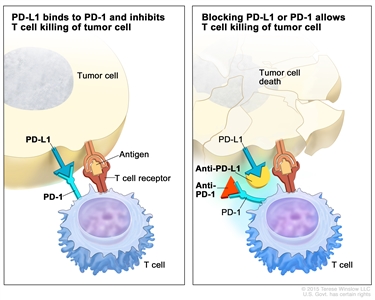
Immune checkpoint inhibitor. Checkpoint proteins, such as PD-L1 on tumor cells and PD-1 on T cells, help keep immune responses in check. The binding of PD-L1 to PD-1 keeps T cells from killing tumor cells in the body (left panel). Blocking the binding of PD-L1 to PD-1 with an immune checkpoint inhibitor (anti-PD-L1 or anti-PD-1) allows the T cells to kill tumor cells (right panel). immune checkpoint inhibitorsImmunotherapy uses the body's immune system to fight cancer. This animation explains one type of immunotherapy that uses immune checkpoint inhibitors to treat cancer.
- Interferon (by injection) may be used to treat squamous cell carcinoma of the skin.
- Topical imiquimod therapy is an immune response modifier that may be used to treat some basal cell carcinomas and is applied to the skin as a cream.
See Drugs Approved for Basal Cell Carcinoma for more information.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells.
- Signal transduction inhibitor therapy: This treatment block signals that are passed from one molecule to another inside a cell. Blocking these signals may kill cancer cells. Vismodegib and sonidegib are signal transduction inhibitors used to treat basal cell carcinoma.
See Drugs Approved for Basal Cell Carcinoma for more information.
Chemical peel
A chemical peel is a procedure used to improve the way certain skin conditions look. A chemical solution is put on the skin to dissolve the top layers of skin cells. Chemical peels may be used to treat actinic keratosis. This type of treatment is also called chemabrasion and chemexfoliation.
Other drug therapy
Retinoids (drugs related to vitamin A) are sometimes used to treat squamous cell carcinoma of the skin. Diclofenac and ingenol are topical drugs used to treat actinic keratosis.
New types of treatment are being tested in clinical trials.
Information about clinical trials is available from the NCI website.
Treatment for skin cancer may cause side effects.
For information about side effects caused by treatment for cancer, visit our Side Effects page.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials supported by NCI can be found on NCI's clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Follow-up tests may be needed.
As you go through treatment, you will have follow-up tests or check-ups. Some tests that were done to diagnose or stage the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back).
If basal cell carcinoma and squamous cell carcinoma recur (come back), it is usually within 5 years of initial treatment. Talk to your doctor about how often you should have your skin checked for signs of cancer.
Treatment of Basal Cell Carcinoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of basal cell carcinoma that is localized may include the following:
- Simple excision.
- Mohs micrographic surgery.
- Radiation therapy.
- Curettage and electrodesiccation.
- Cryosurgery.
- Photodynamic therapy.
- Topical chemotherapy.
- Topical immunotherapy (imiquimod).
- Laser surgery (rarely used).
Treatment of basal cell carcinoma that is metastatic or cannot be treated with local therapy may include the following:
- Targeted therapy with a signal transduction inhibitor (vismodegib or sonidegib).
- A clinical trial of a new treatment.
Treatment of recurrent basal cell carcinoma that is not metastatic may include the following:
- Simple excision.
- Mohs micrographic surgery.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Squamous Cell Carcinoma of the Skin
Treatment of squamous cell carcinoma that is localized may include the following:
- Simple excision.
- Mohs micrographic surgery.
- Radiation therapy.
- Curettage and electrodesiccation.
- Cryosurgery.
- Photodynamic therapy, for squamous cell carcinoma in situ (stage 0).
Treatment of squamous cell carcinoma that is metastatic or cannot be treated with local therapy may include the following:
- Immunotherapy with cemiplimab or pembrolizumab.
- A clinical trial of immune checkpoint inhibitor therapy.
Treatment of recurrent squamous cell carcinoma that is not metastatic may include the following:
- Simple excision.
- Mohs micrographic surgery.
- Radiation therapy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Actinic Keratosis
For information about the treatments listed below, see the Treatment Option Overview section.
Actinic keratosis is not cancer but is treated because it may develop into cancer. Treatment of actinic keratosis may include the following:
- Topical chemotherapy.
- Topical immunotherapy (imiquimod).
- Other drug therapy (diclofenac or ingenol).
- Chemical peel.
- Simple excision.
- Shave excision.
- Curettage and electrodesiccation.
- Dermabrasion.
- Photodynamic therapy.
- Laser surgery.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
To Learn More About Skin Cancer
For more information from the National Cancer Institute about skin cancer, see the following:
- Skin Cancer (Including Melanoma) Home Page
- Skin Cancer Prevention
- Skin Cancer Screening
- Childhood Basal Cell Carcinoma and Squamous Cell Carcinoma of the Skin Treatment
- Cryosurgery to Treat Cancer
- Lasers to Treat Cancer
- Drugs Approved for Basal Cell Carcinoma
- Photodynamic Therapy for Cancer
- Immunotherapy to Treat Cancer
For general cancer information and other resources from the National Cancer Institute, visit:
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of skin cancer. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Adult Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Skin Cancer Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/skin/patient/skin-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389265]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2023-05-15
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.


